Insulin is a crucial hormone responsible for blood sugar management.
It helps with the conversion of sugar to energy, but it requires proper understanding and management.
When I was first diagnosed, it took some time to get my head around the fact that I would be injecting insulin for the rest of my life. I didn’t know anything about the stuff – but I learnt quickly that it’s pretty important to learn and understand the medicine that keeps you alive!
This post will cover what insulin actually is, the difference between basal and bolus insulin, and important tips for storage and safety of insulin.
What is Insulin?
Insulin is a hormone produced by the pancreas which allows glucose to enter cells to be used for energy.
In Type 1 Diabetes, the pancreas no longer produces insulin. This causes high blood sugar levels.
To replace this lost insulin function, diabetics need to self-administer insulin instead.
When people are diagnosed with Type 1 Diabetes, they often leave the hospital with a life-long prescription for insulin pens (and a dream). But during the stress of it all – it can be overwhelming to understand what insulin actually is.
There are generally two types of insulin available: bolus (fast-acting) and basal (long-acting) insulin.
Bolus Insulin
You may have come across diabetics on social media saying the word “bolus” and thought “what are they on about”? I know I have!
Bolus was one of the first words I had to google because I had never really come across it before, especially not in the context of self-administering insulin.
But that’s essentially what it is!
Novorapid/Novolog, Fiasp, Humalog and Lyumjev are all popular types of bolus insulin.
Bolus insulin is fast-acting insulin taken to access the energy from carbohydrates in food to help manage blood sugar levels.
“Bolus” can have two meanings. A bolus can be a dose of insulin, but it can also be a verb to describe the action of administering insulin.
The bolus of insulin might be administered via a fast-acting insulin pen and needle, or via an insulin pump.
The amount of insulin given is calculated based on individual’s insulin to carbohydrate ratio. This can be calculated with the help of a medical professional.
For example, if you are eating lunch with x amount of carbs, you might bolus x units of insulin.
Typically, insulin boluses (is that even the plural? Bolus’s?) are taken before meals, to correct high blood sugars, or both.
Basal Insulin
You may hear basal insulin referred to as “background insulin” – which sums it up nicely.
Basal insulin acts in the background to regulate blood sugar levels by providing a slow, steady release of insulin.
There are a variety of basal insulin types, which may be administered once or twice a day, depending on type.
Lantus, Levemir and Tresiba are all popular types of basal insulin.
You may be required to do something called “basal testing” by your health care provider. This makes sure your basal insulin dose is correct by checking your blood sugar level without the interference of food intake.
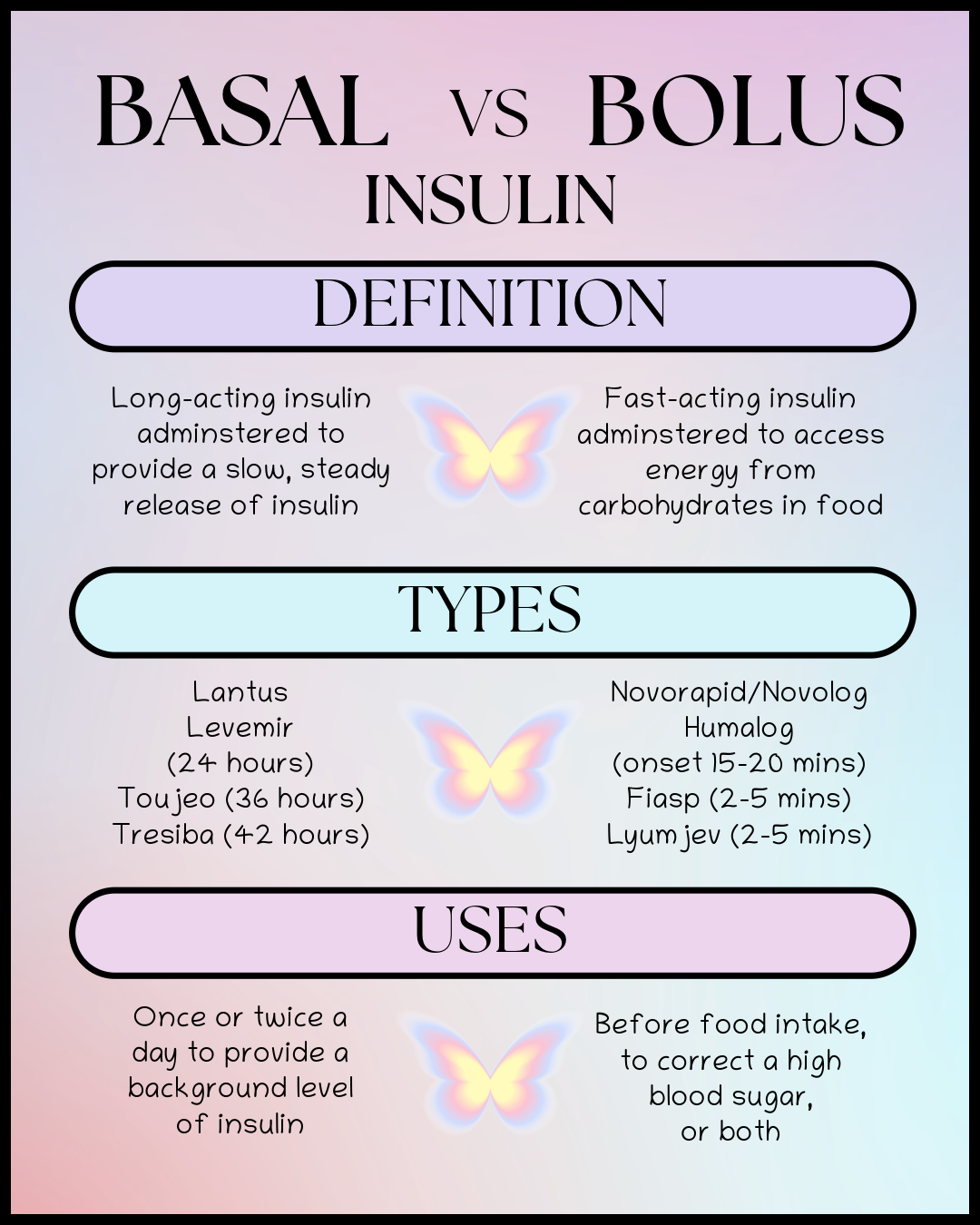
Bolus and Basal
Basal and bolus insulin injections are both necessary to manage blood sugar levels as they complement each other.
Basal handles the body’s background insulin needs, whereas bolus handles the immediate blood sugar spikes from food intake.
The amount of insulin administered as a basal or bolus is extremely personal and unique to every diabetic. Adjusting the amounts of insulin should be done with a healthcare provider’s guidance. You need to learn how to adjust the amount of insulin you need depending on carbohydrate counts, insulin to carb ratio’s, and correction factors. So much fun!
Insulin Storage
Insulin can be a delicate medicine, and so it requires specific storage conditions.
Temperature guidelines:
- Unopened insulin should be stored in the fridge, between 2-8°C or 36-46°F
- Once opened, insulin can stay at room temperature (below 30°C or 86°F)
- Opened insulin remains viable for up to 28 days.
The specific details for your insulin will be on the packaging.
Storage tips:
- Avoid extreme low temperatures. Freezing can damage insulin and prevent it from working. Keep an eye on your fridge to make sure it doesn’t malfunction and freeze everything.
- This happened to me once in my uni house fridge – my yoghurt was frozen solid, and while I was initially sad because I had bolused insulin for it, I was even sadder when it dawned on me that my insulin was also frozen. Queue the emergency prescription request!
- Avoid extreme high temperatures. If insulin gets too hot, it can have reduced efficiency. After all, insulin is a hormone, which is a protein, and proteins denature in hot temperatures.
- I sometimes find that if my insulin has been left out in the sun, or in hot temperatures, I may need a lot more insulin than usual. While this could be because of my own insulin resistance in hot weather, it could also be because the heat has reduced the efficiency of the insulin. Just something to be aware of!
- Never leave insulin in a hot car, or in direct sunlight
Travel Tips
Travelling with Type 1 Diabetes can be a challenge. One of the challenges can include storing insulin.
Under 28 days
For short trips under 28 days, it’s easy to throw a few insulin pens or cartridges into your bag and away you go.
There’s no need to worry about insulin being out of the fridge for under 28 days.
However – you may be travelling somewhere with extreme temperatures. In this case, it may be sensible to store your insulin in a cooler or insulated bag.
Popular brands like Frio are good for keeping insulin cool.
I used the pouches a lot when I was first diagnosed, especially living in hot Texas during summer.
However, I found that keeping insulin out of direct sunlight and inside a backpack, was usually cool enough. So don’t be worried if you don’t splash out on a pouch!
Something like an insulated lunch bag, which you may already have, is ideal for travelling with insulin.
Over 28 days
For longer trips over 28 days, it’s a bit more of a challenge.
Ideally, you can pack your insulin at the very last minute, in an insulated cool bag.
This can keep the insulin cool enough until you reach your destination, and then use the fridge at your accommodation to resume the cold storage.
However, if your travel time is long, this is a bit more difficult.
Personally, when I travelled to Australia, I had two insulated cool bags with ice blocks in both, and a towel layer separating the ice blocks and the insulin. However, my ice blocks were very much melted by the time I was on the plane.
I’ve been using that insulin for the last 7 months and my blood sugars are better than ever, so clearly nothing bad happened!
Of course this is just my experience and not medical advice.
Airport Security
Is insulin a liquid or not?! That is one question I think all of the airports should come together and discuss.
Obviously, insulin is a liquid. But it’s a liquid medicine. So it should go in a liquids bag, right?
Unfortunately this definition is very much airport dependent. The majority of airport security do not care about insulin, and will tell you to keep it in your bag.
Other airports (cough cough Manchester) will make you remove your insulin pens from the cardboard box, and put them into a liquids bag.
Because I am clearly scarred from this experience, I will always put my insulin into a liquids bag.
One time I was heading home from Manchester (shock) and I had two liquids bags: one full of makeup busting at the seams, and another one with insulin and glucose gels in it. The security guard literally scrutinised the contents of my medical bag, and told me that the 2 spare contact lenses I had snuck in there out of desperation were not medical. I mean she did have a point… but still, sue me!!!
In short – tell the security guards you have diabetes supplies and hope they do not care lol.
Again, not medical advice, just my experience.
Insulin Safety Tips
Check expiration dates
Checking the expiry dates on your insulin pens is so important.
When you pick up new insulin you should rotate the stock in your fridge. This makes sure that you are always reaching for the shortest in-date insulin. This means you won’t have to worry that you used up all your insulin with long expiry, and only have insulin that expired last month!
FYI: I learnt during my time working at a pharmacy, if you only have a month and year expiry date, it won’t be expired until the very end of the month. For example “05/2028” means the insulin is fine to use for all of May, but once June hits, it’s expired.
This may be common knowledge but it’s really stuck with me!
Inspect the quality of insulin
Insulin is a clear, colourless liquid. There should be no dust, floaters, specs, cloudiness, or discolouration.
Avoid using poor quality insulin, and start a fresh pen or vial instead.
Proper Injection Techniques
Maintaining good habits when it comes to insulin injections is crucial.
Always rotate injection sites. You can use pretty much any “fatty” part of your body: arms, belly, back/love handles, legs.
By giving sites time to breathe between injections, you reduce the likelihood of lipodystrophy (lumps under the skin). This helps to keep the absorption of insulin consistent.
Avoid injecting in areas which are bruised, or swollen, as insulin may not absorb correctly.
Handling Insulin Pumps
If you are administering insulin via an insulin pump, it’s important to check that everything is functioning as it should, and there are no blockages. Often, the pump will inform you if there is a collusion. In this case, you should perform a site change.
One time, my tube was so tangled, it had somehow formed knots. I couldn’t understand why my blood sugars were going sky high, until I looked at my tubing!
Overall, insulin is a crucial hormone for managing blood sugar levels, and thanks to it’s discovery over 100 years ago, we would be long gone without it! Whether its a basal or bolus, I hope you now understand the importance of proper storage and safety practices.
Please consult your healthcare provider for personalised insulin advice, as I do not provide medical advice – I only share my experiences. So please share your experience with me or ask any questions! I’m always easy to reach on Instagram @lydiabetic
Thank you so much for reading! ❤
Love, Lydia. x
Leave a comment