The term “artificial pancreas” gets thrown around a lot in the world of Type 1 Diabetes. It is often interpreted as something that would be implanted or installed in a Type 1 Diabetic, which would allow them to function as a non-diabetic, and not think twice about it.
Currently, this is far from the truth.
Instead, it is becoming increasingly common for Type 1 Diabetics to use something called Hybrid Closed Loop Technology (HCL).
In a nutshell, HCL systems involve an insulin pump, which can communicate with a continuous blood glucose monitor (CGM), and use the blood sugar level data to constantly adjust insulin delivery to keep blood sugar levels in range.
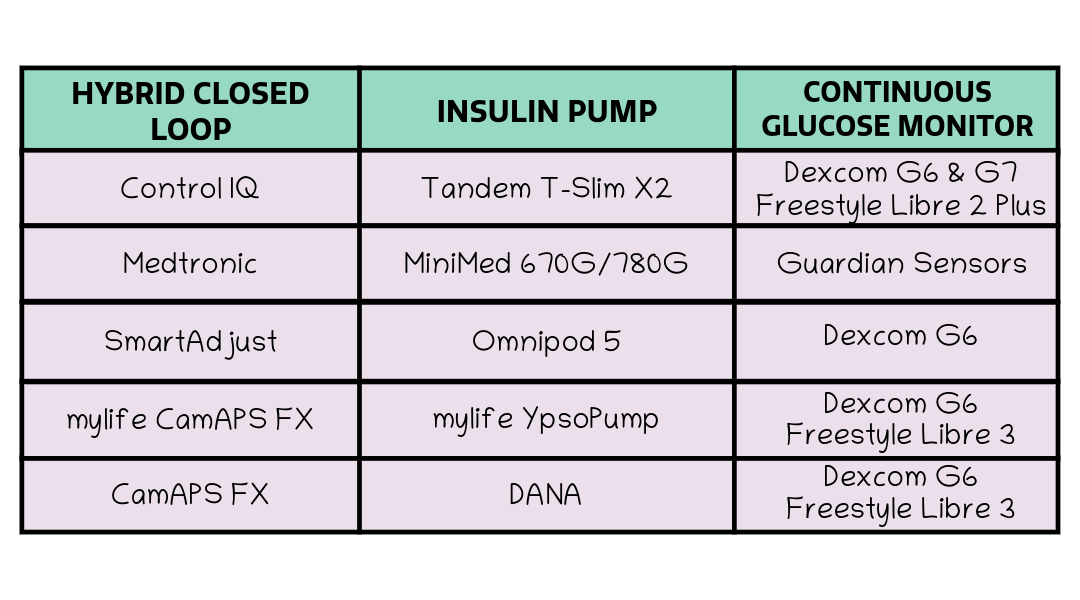
There are a variety of insulin pumps available, such as the Tandem T-slim X2, Omnipod 5, and Medtronic Minimed 770G. These models can communicate with a variety of CGM sensors, such as the Dexcom G6, Dexcom G7, Freestyle Libre 2 Plus, and the Guardian Sensor 3.
HCL’s often get called artificial pancreases, but because they still require human input, such as carb counting, manual insulin pump set changes etc, I am skeptical on the use of the term. I’ll get into it later on, but first off let’s discuss what HCL’s are, and how it all works.
How do you know which HCL system to choose?
Personally, I use the Hybrid Closed Loop system called “Control IQ”. This HCL system is available for use with the Tandem T-slim X2 and Dexcom G7 (as well as the Dexcom G6 and Freestyle Libre 2 Plus).
After spending a lot of time researching my options and comparing insulin pumps, I decided this system was the best for me. You can read my blog post on how I chose my insulin pump here. Overall, I decided the technology and the all-in-one solution a tethered pump provides was my best option.
How Control IQ works
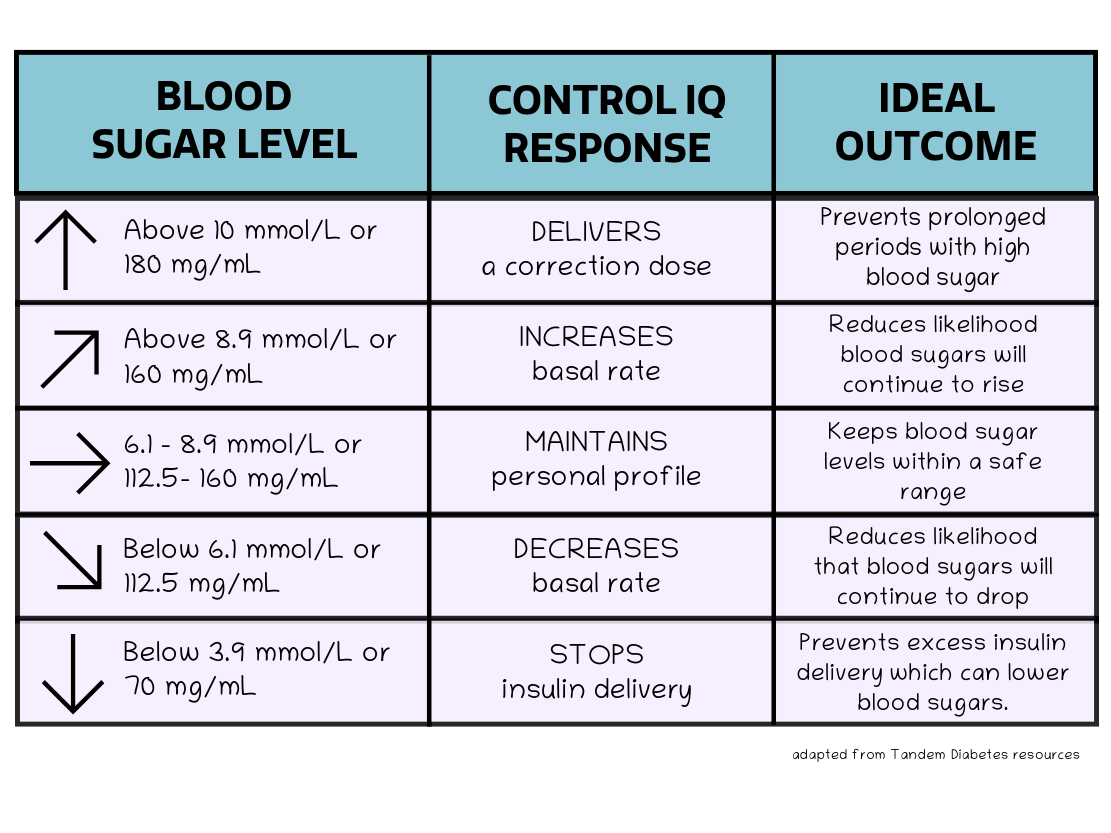
Control IQ constantly adjusts my basal insulin delivery with the aim to maintain my blood sugar level at 6.1 mmol/L. This is considered a safe level to have my blood sugars, which isn’t too high or too low.
If my CGM predicts that my blood sugar will go low (below 4.0 mmol/L), Control IQ will direct my insulin pump to suspend insulin delivery. This is useful because excess insulin delivery can contribute to lower blood sugars, and therefore cause a more severe hypo (low blood sugar). My blood sugar levels might still dip below 4.0, but I am able to treat it with usually a smaller amount of sugar, depending on the circumstances.
If my CGM predicts that my blood sugar will go high (above 10.0 mmol/L), Control IQ will direct my insulin pump to deliver additional insulin. This could be in the form of an increased basal amount, or as a correction bolus. If it is a correction dose, only one can be delivered per hour, to prevent any rapid crashing. But, if levels remain high, the basal can be increased continuously. This increase in insulin delivery is useful to prevent prolonged periods with high blood sugar. This has long term benefits for my health, which will reduce my likelihood of complications in the future.
But how does it know how much insulin to deliver?
When you get an insulin pump, you input your data to create a personal profile. This includes your weight, current basal rate per hour, insulin:carb ratio, etc.
- The basal rate can be calculated by dividing your current daily basal pen injection by 24. The insulin pump will deliver this amount of insulin as a continuous drip. You will probably need to do a few fasted basal tests to make sure it’s right.
- Basal testing involves not eating or drinking anything for a number of hours with no fast acting insulin on board. Ideally, if your basal insulin amounts are correct, your blood sugar will stay in range and steady.
- Calculate your total daily dose (TDD) of insulin by adding your usual background amount of insulin and your average amount of fast acting insulin throughout the day.
- The insulin to carb ratio is calculated based on how many grams of carbohydrates one unit of insulin covers. One method to calculate this is to divide 500 by your total daily dose of insulin. For example, if you have 15 units of Lantus, and 30 units of Novorapid, your TDD is 45, then your insulin to carb ratio is 1 unit:11g carbs.
Control IQ, and other HCL systems, use this data to constantly adjust your basal insulin levels. For example, if your blood sugars are predicted to go high, the Control IQ will increase your basal insulin, but when your blood sugars are coming back down into range, the basal insulin rate will return to normal.
For example, if your basal rate is 1 unit of insulin per hour, once your blood sugars start rising, the rate could be increased to 1.5 units per hour. Once your blood sugars are stabilising again, the rate will be decreased back to 1 unit per hour. In reality, the increase might have only happened for 10 minutes.
Within your personal settings, you can set maximum rates of insulin delivery, to make sure the insulin pump never delivers too much insulin. If you already have insulin on board, for example after a meal, and your blood sugars start to rise, it is unlikely the HCL will deliver any additional insulin immediately. This is because of the maximum rates of insulin delivery. Once the insulin on board has decreased to a suitable level, will the insulin pump begin to deliver extra insulin.
The HCL essentially takes the data that you manually input into your pump profile settings, and learns from that to constantly adjust your insulin delivery.
What are the benefits?
Control IQ has been an absolute game changer for me, and I could sing of its benefits forever! You can read more about my thoughts and feelings on it in my other blog post here.
The big thing for me has been reducing the severity and occurrence of hypo’s (low blood sugar events). These had always been a source of anxiety, and the reason that I micro managed my Type 1 Diabetes to the extreme.
I still have hypo’s, but with the insulin being suspended, they are often not as bad, don’t appear as suddenly or intensely, and can be dealt with a smaller amount of sugar.
Additionally, my sleep has never been better. I am rarely woken by my CGM alarms anymore, whereas this was a nightly occurrence when I was using insulin pens, because God forbid I did a bit of exercise during the day which often made me low in the night!
Instead, the constant adjustment of my insulin delivery throughout the night, with no other stressors, means I often wake up to a blood sugar level of 6.1 mmol/L – ideal!
So is it an artificial pancreas?
In my opinion, no. Hybrid Closed Loops are not artificial pancreases. My idea of an artificial pancreas is one that is completely independent, doesn’t require any human effort, and can work perfectly well on it’s own.
Instead, using a HCL involves constant human imput; counting carbs, pre-bolusing insulin, learning the techniques, changing the pump sites every few days, accounting for exercise, and monitoring blood sugar levels.
I personally think the term “artificial pancreas” over simplifies the technology. It sounds as though the diabetic’s pancreas has been replaced entirely, and they are no longer having to deal with a chronic illness. Doesn’t that sound too good to be true?
To the general public, reading a news article that all Type 1 Diabetics can get an artificial pancreas, might make them think the cure is here and T1D is no longer a burden.
But guess what, T1D is still a menace and blood sugar levels can be erratic, regardless of the hybrid closed loop technology, or “artificial pancreas”.
Of course, the hybrid closed loop system does not know if you have had a high carb meal, if you have exercised, if you inputted the amount of carbs correctly, if your carb ratio is correct, or if you have pre-bolused your insulin. Nor does it know the many other variables that impact our blood sugar.
The technology is definitely a huge advancement and I imagine it will only continue to improve, but for now, there’s a lot of work to be done. Certainly before it can be called a true artificial pancreas.
Why isn’t everyone using this?
Unfortunately, access to this technology is still limited. While the NICE guidelines have recently been updated to include a wider group of people eligible for the technology, the uptake in reality is lacking.
There needs to be more funding into providing the highest standard of care for Type 1 Diabetes, less resistance from the funding bodies who decide who get’s access to the technology, and less of a postcode lottery regarding areas which are “pump friendly” and areas which are not.
Overall, if you are in the privileged position and have the option to access this technology, I absolutely urge you to go for it. I know the idea of a medical device constantly being attached to you is unappealing, but the benefits for improving your standard of life far outweigh any reason not to.
Thank you so much for reading!
Love, Lydia x

Leave a reply to Decoding Diabetes: Understanding Common Terms – LYD1A KERR Cancel reply